Most doctors want to know two things.
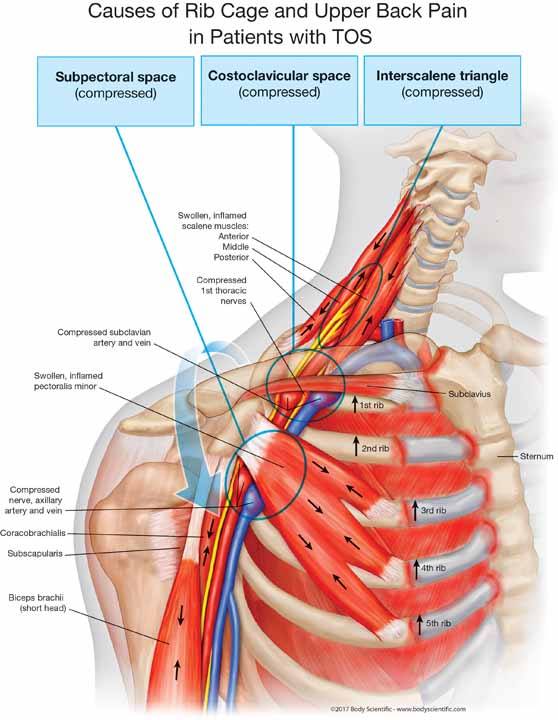
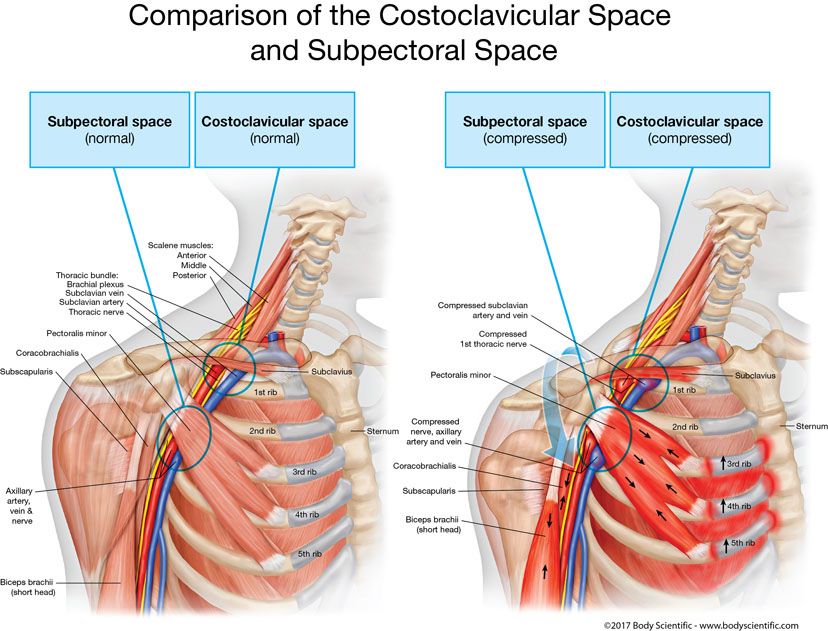
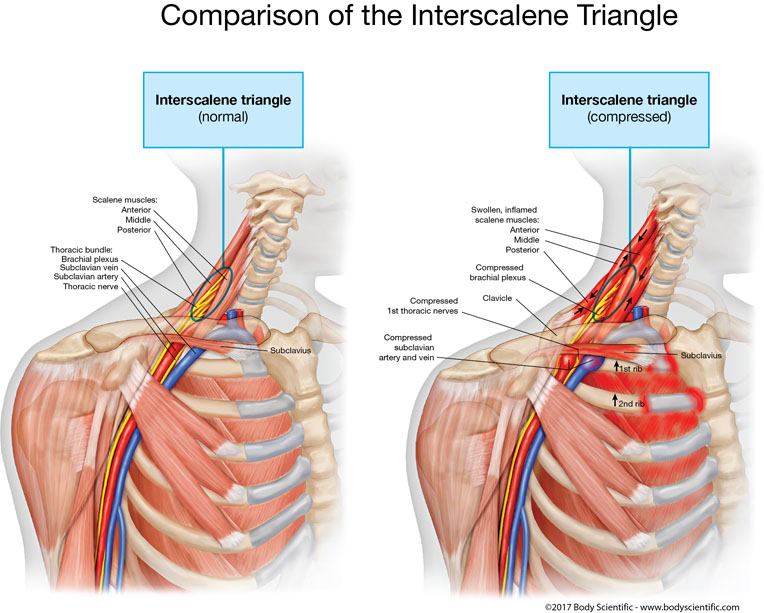
1. Do you have signs of compression of the nerves or blood vessels in the thoracic outlet?
2. What structures in the bundle are compressed—the artery, vein, nerves, or all the above?
In response, investigators have categorized thoracic outlet syndrome as vascular versus neurogenic. Does that mean the artery and vein are compressed or just the nerves? Then they subcategorized as either true or disputed (7).
The four types of thoracic outlet syndromes (determined by what structure of the bundle is compressed) or if they think your diagnosis is wrong
1. True neurogenic TOS—compression of the brachial plexus nerves
2. Arterial TOS—compression of the artery
3. Venous TOS—compression of the vein
4. Disputed neurogenic TOS—assumed compression of the brachial plexus nerves
The problem is that none of this helps them determine what is causing the compression of the outlet. So, they get you to ponder this and many of you obsess over it. When you call me in this desperate situation, telling me you have this chronic severe case of neurogenic or venous thoracic outlet syndrome, I ask you, “Do you really think that the compression of the outlet can isolate the exact blood vessel or nerve that is compressed?”
They spend all this time determining which blood vessel or nerve is compressed, then waste more of your time with treatments that don’t address the cause of the compression. Once I find the muscles that are compressing the outlet, I start the most effective treatment to decompress it to get you the relief you want.
Nerve Compression – Neurogenic TOS
Compression of the Nerves – The most common symptoms of compressed nerves in neurologic thoracic outlet syndromes are pain, numbness, and tingling in 95 percent of cases, of which 90 percent of them are distributed in the inside of the forearm and the last two fingers. When the disc in the neck is herniated, compressing the nerve, it usually shoots pain, causes numbness, and feels tingly in a defined radicular pattern that will suggest to the doctor the exact level of which disc is herniated.
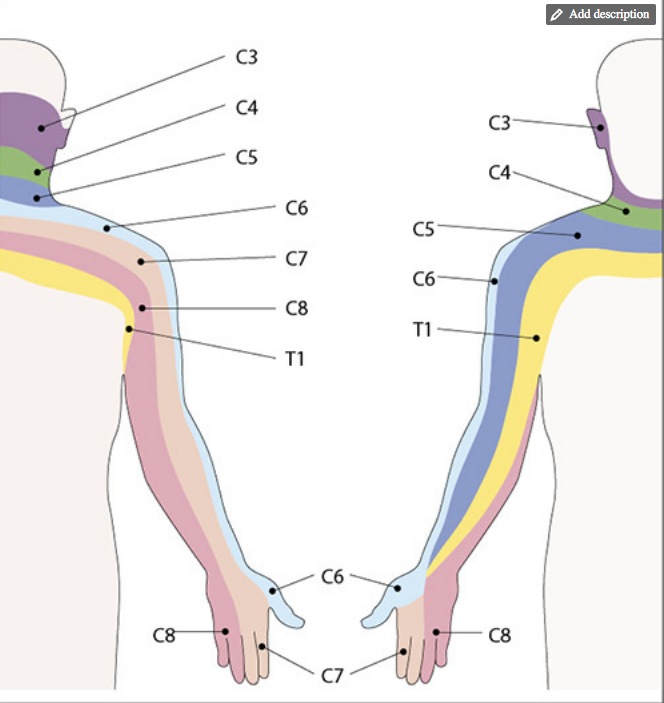
Patients suffering from this condition can present with pain and numbness in an ill-defined distribution (14). With thoracic outlet syndrome, there is either numbness, tingling, or deep pain within the arm. Commonly, I hear patients complain of tingling in the fingertips as the initial symptom. When the rib raises the first nerve, it compresses the nerves that supply feeling to the fourth and fifth fingers.
As the ribs continue to rise from muscle tension, they affect nerves higher up in the brachial plexus. This is when you feel the numbness move from the fourth and fifth fingers to the third, second, and thumb, and then move up the arm. This was the key finding that helped me determine Sonny Burke was misdiagnosed with diabetic neuropathy, because this was the sequence of numbness he had experienced that all his doctors did not pick up.
If you start feeling weakness in grip strength when opening jars or even dropping objects, then you might have a compression of a significant amount of the nerves that supply your arm with feeling and strength. You should get tested with a hand dynamometer. Usually the dominant handgrip strength is 10 percent stronger than the opposite hand grip strength.
Artery Compression (Arterial TOS)
When the rib raises into the artery, the first sign is numbness when performing activities overhead or constant arm movements. The tests for blood flow into the arm, such as the hyperabduction maneuver (Wright’s test), Roos test (elevated arms stress test), and the costoclavicular maneuver will be positive when you are examined by your doctor.
If your arm is pale or lacking color or is a gray color, it is indicative of a compression of the artery, as it cannot get blood to the tissues, which have a lack of oxygen. This causes numbness when mild, and the tissues could be dying or dead in more severe cases.
Patients with blockages of the artery in the thoracic outlet area for arterial obstruction might definitely have cyanosis, cold arms and hands, a gray pallor, and fatigue with exercise, especially in exercise that demands the arms be lifted overhead. Some patients note fatigue after exercise, especially if the arm is elevated during the exertion. Typically, the symptoms occur after exercise instead of during exercise (239).
One interesting test you can have your doctor do is to check your blood pressure on the right arm and the left arm, noting that a difference in blood pressure can mean either thoracic outlet syndrome or that the patient is enduring a lot of stress. Blood pressure can elicit differences (17).
Artery Compression (Arterial TOS)
When the rib raises into the artery, the first sign is numbness when performing activities overhead or constant arm movements. The tests for blood flow into the arm, such as the hyperabduction maneuver (Wright’s test), Roos test (elevated arms stress test), and the costoclavicular maneuver will be positive when you are examined by your doctor.
If your arm is pale or lacking color or is a gray color, it is indicative of a compression of the artery, as it cannot get blood to the tissues, which have a lack of oxygen. This causes numbness when mild, and the tissues could be dying or dead in more severe cases.
Patients with blockages of the artery in the thoracic outlet area for arterial obstruction might definitely have cyanosis, cold arms and hands, a gray pallor, and fatigue with exercise, especially in exercise that demands the arms be lifted overhead. Some patients note fatigue after exercise, especially if the arm is elevated during the exertion. Typically, the symptoms occur after exercise instead of during exercise (239).
One interesting test you can have your doctor do is to check your blood pressure on the right arm and the left arm, noting that a difference in blood pressure can mean either thoracic outlet syndrome or that the patient is enduring a lot of stress. Blood pressure can elicit differences (17).
Disputed Neurogenic TOS—Assumed Compression of the Brachial Plexus Nerves
The disputed or nonspecific-type thoracic outlet syndrome refers to a large group of patients with unexplained pain in the arm, scapular region, and cervical region. Many doctors who work with musculoskeletal conditions feel thoracic outlet syndrome is underdiagnosed (1), some doctors who don’t know how to examine for it say it’s overdiagnosed (2), others say it’s misdiagnosed (3), or not diagnosed (4).
The disputed TOS is when some doctor thinks another doctor’s diagnosis is incorrect, so it is disputed. The patient might have chronic pain in the area of the thoracic outlet that worsens with activity, but the specific cause of the pain can’t be determined.
Let’s say you have a car accident with injuries, and you go to a doctor for an examination. Based on your doctor’s history examination and diagnostic test findings, he or she decides you have thoracic outlet syndrome. Then you are asked to go to a company doctor who is paid for by the insurance company. That doctor does his or her workup and decides your thoracic outlet diagnosis is incorrect, so their diagnosis is disputed neurogenic TOS.
Some doctors don’t think thoracic outlet syndrome exists. Most don’t think it exists until they get it. Patients can present with multiple unilateral or bilateral signs and symptoms associated with involvement of both neurogenic and vascular components.
The bottom line is that naming which blood vessel or nerve is compressed more than another is not important. What is important is to determine what muscles are compressing the outlet then do the work to release them.

Now spring to action! Get the book and start reading, learning and healing today!
This is an excerpt from a chapter in Dr Stoxen’s #1 best seller The Human Spring Approach to Thoracic Outlet Syndrome. The book is available on Amazon.com in these 13 counties US UK DE FR ES IT NL JP BR CA MX AU IN on Kindle. The book is available on Amazon.com in these 7 counties US UK DE FR ES IT JP in paperback.

Dr James Stoxen DC., FSSEMM (hon) He is the president of Team Doctors®, Treatment and Training Center Chicago, one of the most recognized treatment centers in the world.
Dr Stoxen is a #1 International Bestselling Author of the book, The Human Spring Approach to Thoracic Outlet Syndrome. He has lectured at more than 20 medical conferences on his Human Spring Approach to Thoracic Outlet Syndrome and asked to publish his research on this approach to treating thoracic outlet syndrome in over 30 peer review medical journals.
He has been asked to submit his other research on the human spring approach to treatment, training and prevention in over 150 peer review medical journals. He serves as the Editor-in-Chief, Journal of Orthopedic Science and Research, Executive Editor or the Journal of Trauma and Acute Care, Chief Editor, Advances in Orthopedics and Sports Medicine Journal and editorial board for over 35 peer review medical journals.
He is a much sought-after speaker. He has given over 1000 live presentations and lectured at over 70 medical conferences to over 50,000 doctors in more than 20 countries. He has been invited to speak at over 300 medical conferences which includes invitations as the keynote speaker at over 50 medical conferences.
After his groundbreaking lecture on the Integrated Spring-Mass Model at the World Congress of Sports and Exercise Medicine he was presented with an Honorary Fellowship Award by a member of the royal family, the Sultan of Pahang, for his distinguished research and contributions to the advancement of Sports and Exercise Medicine on an International level. He was inducted into the National Fitness Hall of Fame in 2008 and the Personal Trainers Hall of Fame in 2012.
Dr Stoxen has a big reputation in the entertainment industry working as a doctor for over 150 tours of elite entertainers, caring for over 1000 top celebrity entertainers and their handlers. Anthony Field or the popular children’s entertainment group, The Wiggles, wrote a book, How I Got My Wiggle Back detailing his struggles with chronic pain and clinical depression he struggled with for years. Dr Stoxen is proud to be able to assist him.
Full Bio) Dr Stoxen can be reached directly at teamdoctors@aol.com