Why must your doctor know the biomechanics of your human springs to treat you for thoracic outlet syndrome?
What is the evidence that your doctor does not use biomechanics in the treatment of your thoracic outlet syndrome?
Clue 1 – Your doctor doesn’t take the time to ask you detailed questions about activities of your daily life that could be triggering your thoracic outlet syndrome.
Clue 2 – Your doctor gives you a prescription for a chemical, a painkiller, or an anti-inflammatory drug, when your problem is mechanical.
Clue 3 – The doctors order an MRI, based on your symptoms, instead of a full thorough examination. They don’t touch you where it hurts.
Bioengineering
The science of bioengineering is the use of artificial tissues or components to replace damaged or absent parts of the body, such as artificial limbs. The push to continually improve the outcome of total joint replacements and limb replacements eventually led orthopedic surgeons to pay more attention to biomechanics and bioengineering to better understand how the body moves.
The irony is that doctors work harder on understanding biomechanics so they can develop better hip and knee replacements, instead of understanding biomechanics that leads to the compression of the joints, which is the cause of the degeneration. There is more money in the replacements than the prevention.

Most important, doctors need to know how the thoracic outlet remains open and what controls the tension that closes it down. Simple anatomy has been the foundation of medical education, intervention, and communication for hundreds of years. With all the resources multiplying on the Internet, doctors should have a better grasp of anatomy than in the days I went to school, when we learned by dissecting a cadaver with the help of a paperback guide.
But in fact, doctors are having a more difficult time understanding simple anatomy, specifically the anatomy of the thoracic outlet. That is because, in recent years, human anatomy has been slowly squeezed from the medical curriculum. Some suggest that it has fallen below a safe level.
Not only is there evidence that doctors are not learning enough anatomy to provide effective care, there is evidence that the lack of knowledge of anatomy has caused medicine to be a less safe practice for patients.

Between 1995 and 2000, there was a seven-fold increase in malpractice claims associated with anatomical errors submitted to the United Kingdom Medical Defence Union (MDU), and 32 percent of claims, in general, made to the MDU. Malpractice claims for vascular surgery were reported most commonly for “damage to underlying structures” during surgery (1).
This is incredibly important, considering that vascular surgeons are the specialists called to do the surgery for thoracic outlet syndrome. They are expected to remove clots, repair blood vessels, cut out scalene muscles of the neck and the pectoralis minor muscle of the shoulder and chest, and surgically remove the first rib, all without causing damage to underlying structures. There are a lot of tiny nerves and blood vessels in the neck, chest, and shoulder.
Doctors’ over reliance on MRIs to diagnose demonstrates they don’t understand the body as an interconnected mechanism. They use chemicals to treat the body, when the problem is mechanical.
People keep defending these physicians saying, “That’s how they do it, according to the way they were taught or believe.” If the way they do it leaves you in chronic pain for life, then it is an incorrect way to approach thoracic outlet syndrome. Period!
When you think about it, these doctors are really not engineers of the body, but merely technicians who know how to remove fluids, put fluids back in, and replace parts when they are worn out. The fact is that hospitals would rather employ technicians who act as minions to carry out procedures that generate huge incomes, rather than thinkers, because the employed technicians will generate more income for the hospital.
So, if your doctor isn’t going to learn this, you have to learn it yourself.
When you go to a personal trainer and ask, “What book would you recommend to learn how to train the body?” most well-educated trainers will ask you to qualify your goals. “Do you want to do resistance exercise or plyometric training?” Resistance exercise uses levers, while plyometric exercise uses the body’s spring mechanics.

Obviously, both are different. So, which one is the right one?
Both are right.
The trainer is just developing one system over the other. Next time, ask your trainer to train the spring system and hand him or her a copy of this book.
Most doctors give you the owner’s manual, describing how you move by levers. What they give you is only half the owner’s manual—lesson one. This chapter you are reading now will be the second half of your owner’s manual—lesson two—which is most important, because it provides an explanation of the spring engineering of the thoracic outlet.
In this chapter, you will come to recognize, beyond doubt, that the current model of how doctors think the body is engineered, the lever model, is a 340-year-old outdated model that doesn’t comply with even the most basic common-sense scientific principles.
Then, I am going to present you with the new, more logical, model of human engineering that has garnered me invitations to lecture all over the world at prestigious medical conferences.
We need these questions answered to determine how the body is engineered.
To understand the cause of any particular musculoskeletal-related condition, including thoracic outlet syndrome, we need to look at how the body is engineered. To better understand that, we must look at how it lives in harmony in a world governed by the laws of basic physics and nature. These are some important questions to answer about engineering and the human body.
How is the body designed or engineered?
- How is it engineered to protect itself from impacts or collisions during simple walking?
- How is it designed to recycle energy for maximum efficiency?
- How is it engineered to provide spaces, so joints won’t bang or grind down?
- How is it engineered to provide safe passage of blood vessels and nerves through spaces or tunnels, like the thoracic tunnel or outlet?
Then, we must consider these questions of how the tension of the mechanism is controlled?
That will give us the answers to how this marvel of engineering becomes compressed, causing thoracic outlet syndrome and a dozen or more other conditions that doctors find difficult to treat.
Human Spring Model Explains the Mysteries that the Lever Model Cannot
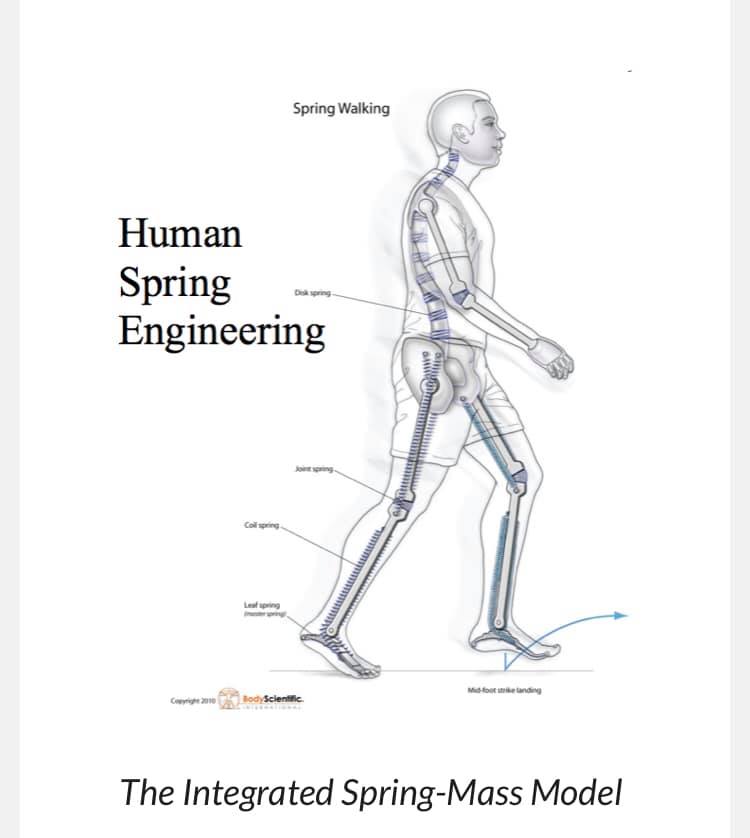
1. The human spring model demonstrates the lower limbs and spine as torsion springs that spring the body back from collisions.
This is like the advancement from the old shocks that cars had in the early days to the torsion bar suspension, also known as torsion spring suspension. It is a general term for any vehicle suspension that uses a weight-bearing spring that is a compression spring and a spring that absorbs stress with a twisting, spring-like motion.
A demonstration of how a torsion spring works occurs when you ring out a wet towel. When you ring it out, the towel changes it shape and stores energy. Then when you release it, it unwinds to its original shape, releasing energy. That is a simple torsion spring.
2. The human spring model extends the spring engineering beyond the legs to model the spine as a torsion spring composed of compression springs, which are the discs between the vertebrae.
Because we have extended the model to the head, we can now understand how to study the areas where thoracic outlet syndrome develops. It also allows us to develop better approaches to examination, treatment, and preventions of conditions, such as herniated discs in the neck too, so if the treatment I outline here is effective for thoracic outlet syndrome, it is equally effective for herniated discs in the neck.
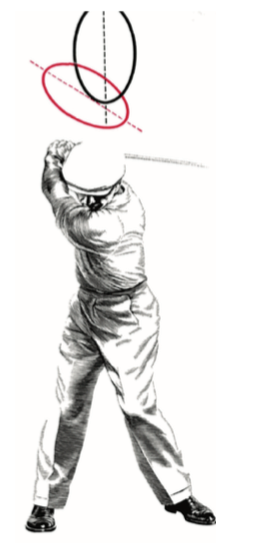
More important, it is a better model to be able to predict what postures and repetitive movements will cause friction, strain, and compression of your body’s spring. For this, we have to understand better how the nervous system controls tension on the spring with various standing and sitting positions in addition to various movements.
Human Spring Model Explains the Mysteries that the Lever Model Cannot

1. The human spring model demonstrates the lower limbs and spine as torsion springs that spring the body back from collisions.
This is like the advancement from the old shocks that cars had in the early days to the torsion bar suspension, also known as torsion spring suspension. It is a general term for any vehicle suspension that uses a weight-bearing spring that is a compression spring and a spring that absorbs stress with a twisting, spring-like motion.
A demonstration of how a torsion spring works occurs when you ring out a wet towel. When you ring it out, the towel changes it shape and stores energy. Then when you release it, it unwinds to its original shape, releasing energy. That is a simple torsion spring.
2. The human spring model extends the spring engineering beyond the legs to model the spine as a torsion spring composed of compression springs, which are the discs between the vertebrae.
Because we have extended the model to the head, we can now understand how to study the areas where thoracic outlet syndrome develops. It also allows us to develop better approaches to examination, treatment, and preventions of conditions, such as herniated discs in the neck too, so if the treatment I outline here is effective for thoracic outlet syndrome, it is equally effective for herniated discs in the neck.
More important, it is a better model to be able to predict what postures and repetitive movements will cause friction, strain, and compression of your body’s spring. For this, we have to understand better how the nervous system controls tension on the spring with various standing and sitting positions in addition to various movements.
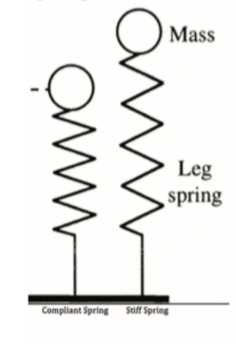
3. The human spring model shows the head as a mass that balances on top of the spring.
The head is modeled as a bowling ball structure that balances precariously on top of a six-story torsion spring. This might give you a better appreciation of how the positions of the head and arms effect the tension on the spring and the thoracic outlet tunnel.
We can use the laws of physics (gravity), the laws of nature (spring weakness versus spring strength), and the understanding of how the brain patterns repetitive postures and patterns of movement to determine how your spring can be expanded, for injury protection, or how it can become compressed, leading to increased risk of injury.
This would explain how you acquired thoracic outlet syndrome and why it won’t go away.
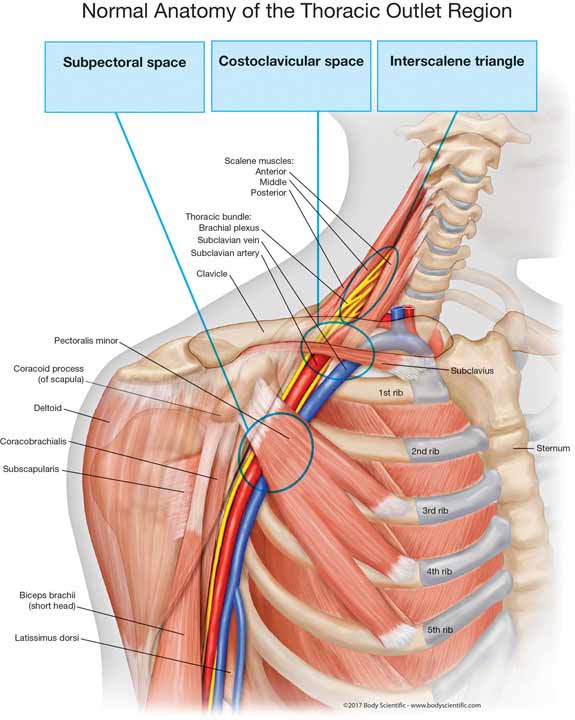
4. The human spring model provides the shoulder with suspension springs that form the outlet and tunnel for blood vessels and nerves to pass.
Your shoulder is suspended from above by muscles that attach at the neck, forming a tunnel, which provides a safe passage for the nerves and blood vessels. There are other opposing muscles that pull your shoulder down into the tunnel. Understanding this will give us a clear understanding about the muscles to treat to release the compression from the outlet and the muscles to strengthen to help better suspend the shoulder higher so that you have a wider and stronger outlet and tunnel.
In the integrated spring mass model, your entire body is one giant spring, composed of multiple floors of springs. In fact, millions of tiny springs, such as muscle fibers, ligaments, and tendon fibers act as rubber bands to load energy in and elastically spring back the energy.
There are extension springs that suspend body parts, compression springs that bounce body parts off one another, and even elastic, balloon-like springs that help your heart beat and your chest expand and contract allowing you to breathe easier.
This is the key to understanding how I can run barefoot for miles on solid concrete at age 53. It also explains how top athletes can collide head-on and neck first at top speeds and not suffer injuries to the thoracic outlet area, yet you are sitting quietly at your desk without trauma and your thoracic outlet is severely compressed, causing excruciating chronic pain and suffering.
How the body is designed as a spring mechanism, how the nervous system modulates tension, and how too much tension on your spring can affect human performance was the subject of the presentation I gave at the World Congress in Sports and Exercise Medicine on August 26, 2014, in Kuala Lumpur, Malaysia. The title of the lecture was, “How Athletes, Coaches, Trainers and Physicians Can Improve Human Performance by the Earliest Detection, Intervention and Prevention of Spring Stiffness Over Modulation.”
On September 4, 2015, I gave the keynote presentation, “The Sports Medicine’s Approach to Anti- Aging Medicine,” at the Seventh Annual Thailand Congress on Anti-Aging and Aesthetic Medicine, held in Bangkok, Thailand. You can watch the entire presentation online here….
You can also find the video of the lecture, “The Integrated Spring-Mass Model to Understanding the Earliest Detection, Intervention, and Prevention of Thoracic Outlet Syndrome,” I gave for the A4M Thailand World Congress on Anti-Aging Medicine, 2017.
In the presentation, I expanded on this concept of over activity or over control of the nervous system, which leads to compression of the human spring mechanisms. It is the most likely cause of degenerative arthritis and chronic compressive disorders, such as thoracic outlet syndromes, herniated discs, and many other conditions.
Once you learn the secrets to human spring engineering, you will begin to solve the mysteries of many chronic conditions, disorders, and diseases. There are more clues to the mysteries, which will be answered in the next two chapters.
Now spring to action! Get the book and start reading, learning and healing today!
This is an excerpt from a chapter in Dr Stoxen’s #1 best seller The Human Spring Approach to Thoracic Outlet Syndrome. The book is available on Amazon.com in these 13 counties US UK DE FR ES IT NL JP BR CA MX AU IN on Kindle. The book is available on Amazon.com in these 7 counties US UK DE FR ES IT JP in paperback.
Order your copy and start reading and healing today.



Dr James Stoxen DC., FSSEMM (hon) He is the president of Team Doctors®, Treatment and Training Center Chicago, one of the most recognized treatment centers in the world.
Dr Stoxen is a #1 International Bestselling Author of the book, The Human Spring Approach to Thoracic Outlet Syndrome. He has lectured at more than 20 medical conferences on his Human Spring Approach to Thoracic Outlet Syndrome and asked to publish his research on this approach to treating thoracic outlet syndrome in over 30 peer review medical journals.
He has been asked to submit his other research on the human spring approach to treatment, training and prevention in over 150 peer review medical journals. He serves as the Editor-in-Chief, Journal of Orthopedic Science and Research, Executive Editor or the Journal of Trauma and Acute Care, Chief Editor, Advances in Orthopedics and Sports Medicine Journal and editorial board for over 35 peer review medical journals.
He is a much sought-after speaker. He has given over 1000 live presentations and lectured at over 70 medical conferences to over 50,000 doctors in more than 20 countries. He has been invited to speak at over 300 medical conferences which includes invitations as the keynote speaker at over 50 medical conferences.
After his groundbreaking lecture on the Integrated Spring-Mass Model at the World Congress of Sports and Exercise Medicine he was presented with an Honorary Fellowship Award by a member of the royal family, the Sultan of Pahang, for his distinguished research and contributions to the advancement of Sports and Exercise Medicine on an International level. He was inducted into the National Fitness Hall of Fame in 2008 and the Personal Trainers Hall of Fame in 2012.
Dr Stoxen has a big reputation in the entertainment industry working as a doctor for over 150 tours of elite entertainers, caring for over 1000 top celebrity entertainers and their handlers. Anthony Field or the popular children’s entertainment group, The Wiggles, wrote a book, How I Got My Wiggle Back detailing his struggles with chronic pain and clinical depression he struggled with for years. Dr Stoxen is proud to be able to assist him.
Full Bio) Dr Stoxen can be reached directly at teamdoctors@aol.com























